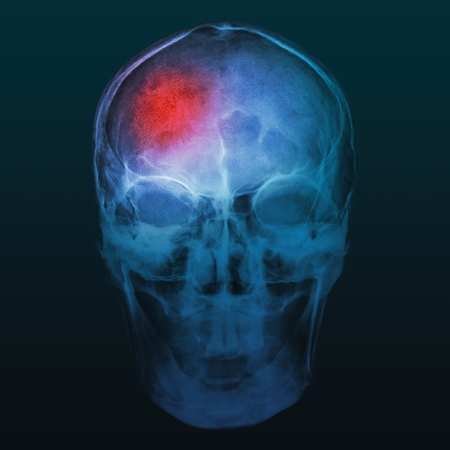
Stroke
Stroke, in general terms, is any sudden vascular injury to the brain. It represents one of the biggest killers in the world. In Australia, a new stroke is estimated to occur once every nine minutes. Stroke can be divided into 2 main types: Ischaemic strokes (where there is a blockage in a blood vessel supplying oxygen and nutrients to the brain); or Haemorrhagic strokes (where there is bleeding into the brain tissue itself). Approximately 80% of strokes are due to blockage, while 20% are due to bleeding. In case of ischaemic stroke, damage to the brain from stroke can potentially be reversed if blood flow is restored within a short period of time. Every minute the brain is deprived of blood, 2 million brain cells or neurons die (or permanently damaged) and cannot be replaced. Therefore, there is a motto: Time is Brain! Recent innovations in medical science have allowed neuro-interventional surgeons to reopen blood vessels that are blocked for up to 24 hours, and be able to improve outcomes on stroke patients. (See Stroke – Endovascular Clot Retrieval). A number of risk factors can lead to increased risks of developing strokes, and some of these are preventable.
Causes
Ischaemic Strokes (Blockage in brain artery) can be caused by:
- Plaque in neck artery (commonly carotid artery) – Build-up of cholesterol plaque within the arterial wall can lead to narrowing, which can become unstable and break off to travel downstream or embolise to block arteries in the brain, leading to oxygen deprivation, stroke and permanent brain damage. Factors that promote plaque formation include: Smoking, high blood pressure, diabetes, high cholesterol, family history. Control of these factors and aspirin may decrease risk of stroke.
- Irregular heart rhythm (‘cardiac arrhythmia’, such as atrial fibrillation) – Irregular heart rhythm can lead to formation of clots within the heart chambers. Atrial fibrillation is a common heart rhythm disorder that increases the risk of strokes up to 6% per year. Clots from the heart can travel or embolise to brain arteries, also causing oxygen deprivation, stroke and permanent brain damage. Blood thinners, such as warfarin, clexane or novel oral anti-coagulant agents (NOAC) can decrease risk of strokes.
- Mechanical heart valves – increase the risk of clot formation on the artificial heart valves. High dose blood thinners, such as warfarin, clexane or NOAC can decrease risk of ischaemic strokes.
- Haemorrhagic Strokes (Bleeding into brain tissue) can be caused by:
- Uncontrolled high blood pressure – Sustained or long-term high blood pressure can lead to changes in the vessel wall of small arteries in the brain, which can become weak and cause bleeding. These bleeds typically tend to be in the deeper portions of the brain, which become permanently damaged, and may not be easily removed by surgical means. Vascular abnormalities, such as brain aneurysms, brain AVMs or dural arteriovenous fistulas. These are neurovascular conditions that have increased bleeding risk. To learn more, see brain aneurysms, brain AVMs, dural arteriovenous fistulas and carotid-cavernous fistulas.
- Amyloid angiopathy – An uncommon condition that occurs in the elderly that increases the risk of bleeding in the front (frontal lobe) and back portions (occipital lobe) of the brain.
Symptoms
Stroke symptoms occur suddenly, and may involve any of the following:
- Weakness – usually one side of the body, involving the face, arm and leg; occasionally, both sides can be affected or ‘crossed’.
- Numbness – affecting one of the body, involving face, arm and leg.
- Visual changes – this can result in blurred vision in one eye (‘amaurosis fugax’) or both eyes, or double vision.
- Speech changes – this can result in slurring of speech (‘dysarthria’) or confused / incomprehensible speech (‘dysphasia’).
- Sudden loss of consciousness.
- Sudden severe headaches.
- Dizziness.
- Unexplained falls.
Early recognition is vital because every minute counts. An easy way to remember the signs of stroke are: F – Face: Check the face, has the mouth drooped? A – Arm: Lift both arms, does one side sag? S – Speech: Is the speech slurred? Can they understand you? T – Time: Time is critical. If any of these signs are present, call an ambulance.
Tests / Diagnosis
Anybody with symptoms of stroke as described above should be transferred urgently by ambulance to an emergency department, preferably in a stroke centre. Urgent assessment with physical examination, and CT (computed tomography) scan of the brain will be performed. CT scan will determine if the stroke is likely to be ischaemic or haemorrhagic. Other tests that may be performed to assess ischaemic strokes include: CTA (CT angiography) and CTP (CT perfusion), which will determine if there is a blockage in a large blood vessel supplying the brain, the amount of brain tissue already lost, and the amount at risk of permanent damage if blood flow is not restored. At other times, MRA (magnetic resonance angiogram) or MR perfusion may also be performed. For haemorrhagic strokes, usually an additional CTA is sufficient to rule out an aneurysm or brain AVM. DSA (digital subtraction angiography) or cerebral angiogram may be performed, either to rule out other causes for haemorrhagic stroke, or as part of further treatment of the stroke, e.g. Endovascular clot retrieval for acute stroke vessel blockage, or endovascular treatment of aneurysms or brain AVMs.
Treatments
Treatment for stroke involves a multi-disciplinary team of: Stroke doctors (neurologists, neuro-interventional surgeons, intensive care specialists), nurses, stroke care coordinators, allied health professionals (physiotherapists, occupational therapists, speech pathologists, psychologists, dietitian, pharmacists), rehabilitation specialists and primary care doctors / GPs. There are many stages or facets to stroke treatment:
- Initial treatment – The focus in the first 24 – 48 hours is to minimise the damage to the brain by restoring blood flow if possible in ischaemic strokes, reducing resultant brain swelling from stroke and intensive monitoring, in case, additional neurosurgical procedures are needed (e.g. hemicraniectomy). For haemorrhagic strokes, removal of the blood clot and releasing the pressure within the brain may be required with a neurosurgical operation.
- Rehabilitation – Once the critical period is over, the focus shifts to restoring function. Allied health professionals and rehabilitation specialists will work closely with patients to achieve maximum recovery after the stroke (including thinking, memory, communication, continence issues, mobility, emotions, coordination).
- Secondary prevention – This addresses the underlying cause for the stroke or any risk factors that may lead to a second stroke in the future. Correction of high blood pressure, cholesterol, diabetes, stopping smoking, starting blood thinners and other medications are key to prevention. Sometimes, where the stroke is caused by narrowing in the neck arteries, an operation is performed to clear the plaque (carotid endarterectomy or carotid artery stenting). If the stroke was due to a neurovascular condition, such as brain aneurysm, brain AVM or dAVF or CCF, these will be treated by the neurosurgeon, either with open microsurgical or endovascular methods.
Related Information
Stroke – Endovascular Clot RetrievalCarotid Endarterectomy & Carotid Artery StentingBrain AneurysmsAneurysms – ClippingAneurysms – Coiling and Stent